Abstract
Adult T-cell acute lymphoblastic leukemia (T-ALL) is an aggressive hematologic malignancy characterized by limited therapeutic options and a high rate of treatment failure due to chemoresistance. T-ALL is largely driven by activating NOTCH1 mutations, where oncogenic NOTCH1 facilitates glutamine oxidation, induces metabolic stress, and facilitates reliance on oxidative phosphorylation (OXPHOS)1. In other malignancies, the shift toward OXPHOS-dependent high-energy status is associated with acquired chemoresistance.
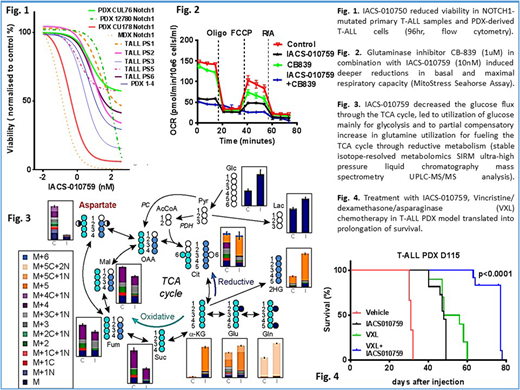
In this study, we found that the novel inhibitor of mitochondrial complex I (OXPHOSi) IACS-0107592 has preclinical activity in NOTCH1-mutated T-ALL; we also characterize the cellular and metabolic responses to OXPHOS inhibition and propose that an OXPHOSi be incorporated into standard-of-care therapy to improve outcomes in patients harboring NOTCH1-mutated T-ALL.
Exposure to IACS-010759 (0-370 nM) in vitro drastically reduced T-ALL viability, with EC50 ranging from 0.1-10 nM for cell lines (n=7) and from 13-60 nM for patient-derived xenograft (PDX)-derived and primary T-ALL cells (n=10) (Fig.1). Oral administration of IACS-010759 (7.5 mg/kg/day) significantly reduced leukemia burden and extended overall survival (p<0.0001) in two aggressive NOTCH1-mutated T-ALL PDX models and in a murine NOTCH1-driven T-ALL model (Fig.4). Addition of OXPHOS inhibitor to dexamethasone (X), vincristine (V), asparaginase (L), or a combination (VXL) led to additive/synergistic inhibition of cell proliferation in vitro and to doubling of overall survival in vivo (p<0.0001) (Fig.4). Metabolic characterization confirmed that IACS-010759 caused striking dose-dependent decreases in basal and maximal oxygen consumption rates (OCR) and ATP and NADH production in T-ALL cell lines and primary T-ALL samples (p<0.001; Fig.2). Further, pretreatment with V, X, or L shifted T-ALL cell metabolism toward OXPHOS, increasing significantly the OCR that was effectively inhibited by IACS-010759. Pharmacological inhibition of complex I with IACS-010759, similar to knockout of complex I subunit NDUFS4 using CRISPR-CAS9, induced catastrophic changes in mitochondria, with induction of mitochondrial reactive oxygen species (ROS), DNA damage, and activation of the compensatory mTOR pathway. OXPHOS inhibition altered cellular energy homeostasis through reduction of TCA cycle intermediates; decreased glutathione level (by UPLC-MS/MS; p<0.0001) with ROS induction (Fig.3); and depleted the pool of intracellular nucleotides, affecting DNA and RNA synthesis (Fig.2C). Stable isotope-resolved metabolomics (SIRM) flux analysis showed that IACS-010759 (30 nM at 24 h) significantly decreased the flux of glucose through the TCA cycle and redirected it toward lactate production and increased utilization of glutamine for fueling the TCA cycle, in particular through reductive metabolism, uncovering reliance on glutaminolysis as an additional therapeutic target. Consistent with this was the finding that combined OXPHOSi with glutaminase inhibitor CB-839 caused additive reduction of viability of T-ALL cells lines and primary T-ALL cells in vitro (Fig.2), decreased tumor burden (p<0.02), and increased survival in a T-ALL PDX model (p<0.01). This was supported by IACS-induced reduction of tumor burden in a NOTCH1-mutated GLS fl/fl murine model upon tamoxifen-induced GLS knockout (p<0.01).
In summary, our findings indicate that OXPHOSi, alone and particularly in combination with standard chemotherapy and GLS inhibition, constitutes a novel therapeutic modality that targets a unique metabolic vulnerability of NOTCH1-mutated T-ALL cells.
References:
Kishton RJ, Barnes CE, Nichols AG at al., AMPK Is Essential to Balance Glycolysis and Mitochondrial Metabolism to Control T-ALL Cell Stress and Survival, Cell Metabolism, 2016, 23(4):649-62
Molina JR, Sun Y, Protopopova M et al., An inhibitor of oxidative phosphorylation exploits cancer vulnerability, Nat Med, 2018, 24: 1036-1046
Lorenzi:NIH: Patents & Royalties; Erytech Pharma: Consultancy. Konopleva:Stemline Therapeutics: Research Funding.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal